Here’s What You Need To Know
Few injuries are as frustrating as knee injuries, especially when you’re left sidelined from your favourite sporting activities. Unfortunately, anyone can fall victim to knee injuries regardless of whether they are professional athletes or regular fitness enthusiasts. In fact, knee injuries can also arise from everyday activities or accidents.
According to a 2006 study, approximately 40% of sports injuries comprise injuries related to the knee joint. But don’t worry, because fixing knees is my specialty. I’ve studied their design, how they function, common injuries, the most cutting edge prevention techniques, and what leading physiotherapists are doing to rehabilitate knee injuries.
Regardless of whether your knee injury stems from patellofemoral pain syndrome, ligament sprains or tears, cartilage tears, tendinitis, or just plain old wear and tear (arthritis), this playbook will explain everything to you and offer tips on how you can prevent them.
If you’ve ever suffered from a knee injury, then this is the article for you to learn more about how you can keep your knees as healthy as possible.
If you’ve never had a knee injury before, this article is also for you. By following the injury prevention tips here, your chances of sustaining a knee injury will be greatly lowered.
Types Of Knee Injuries
Before that, you should know a little bit about the anatomy and inner workings of the knee joint in order to understand the different injuries that may occur. The bones at the knee joint consist of the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The ligaments, which are fibrous connective tissue connecting the bones, help provide joint stabilisation.
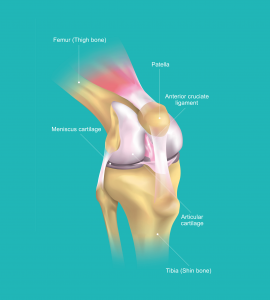
Here’s a quick guide to help visualise the bones which make up your knee:
- The femur: runs from your thigh to your knee
- The tibia: runs from your knee to your ankle
- The patella: the triangular-shaped bone in front of the knee
Now let’s take a closer look at the muscles, tendons, and cartilages that make up the knee joint.
The medial collateral ligament (MCL) provides a form of restraint against valgus forces (anything bent or twisted away from the midline) to the knee. The lateral collateral ligament (LCL), however, provides restraint to varus forces (the opposite of valgus forces) at the knee. These two collateral ligaments are responsible for controlling the sideways motion of your knee and bracing it against unnatural movement.
Next, the anterior cruciate ligament (ACL) serves as the primary restraint to anterior tibial translation on the femur. The posterior cruciate ligament (PCL), on the other hand, limits posterior tibial translation on the femur. Both of these ligaments cross inside the knee joint, thus earning the name ‘cruciate’ (cross-shaped). More importantly, they help to stabilise the knee from the back and the front.
There are many different knee injuries. These can be categorised into broken bone injuries (fractures), soft tissue injuries (dislocations, sprains, ACL injuries, PCL injuries, collateral ligament injuries, meniscal tears, and tendon tears), and overuse injuries that build up over time (arthritis).
ACL Injuries
An ACL injury is essentially a tear or sprain of the anterior cruciate ligament (ACL), which is the ligament that connects your femur to your tibia.
Many patients have reported hearing a ‘pop’ sound coming from their knee upon sustaining an ACL injury. This type of injury is most common in intermittent sprint sports which involve sudden changes in direction, such as basketball, hockey, American football, soccer, and rugby amongst others. However, ACL injuries can also occur from accidents such as falling from a height which places sudden pressure on the knee in an awkward position.
A good number of ACL injuries also come with accompanying damage to other structures in the knee, such as the cartilage, meniscus, and other ligaments. ACL injuries are graded on a severity scale:
- Grade 1 Sprains: Ligament has been stretched, resulting in mild damage. However, the knee joint is still stable.
- Grade 2 Sprains: Ligament is stretched until it has become loose. This is commonly referred to as a partial ACL tear.
- Grade 3 Sprains: Ligament has been split into two pieces, resulting in loss of stability at the knee joint. This is also known as a complete ACL tear.
Causes
There are a number of specific movements that can put stress on the knee, resulting in an ACL injury. These include:
- A sudden stop or change in direction
- Receiving a blow to the knee during a tackle, resulting in hyperextension or inward bending
- Pivoting sharply with one foot firmly planted
- An awkward landing from a jump
Although sports injuries are the common cause of ACL injuries, other patients have also sustained such injuries during car accidents or other trauma, such as falling down the staircase.
Symptoms
Patients who experience an ACL sprain or tear are likely to report some combination of the following symptoms:
- Sharp and intense pain
- Rapid swelling
- Deep aching pain in the knee
- Knee instability
- Loss of full range of motion
Knee Fractures
A knee fracture is a damage to any of the four leg bones which meet at the knee. This includes the patella, the femur, the tibia, and the fibula. Knee fractures can be as mild as a small hairline crack in the bone, or as severe as a complete break.
Orthopaedic surgeons categorise fractures in several ways:
- Non-displaced fracture: Broken pieces of bone remain in contact with each other.
- Displaced fracture: Bone pieces are out of position and no longer aligned.
- Comminuted fracture: Bone breaks into many pieces.
- Open or closed fracture: Denotes whether the bone has broken through the surface of the skin (open) or not (closed).
Knee fractures are typically caused by direct trauma to the knee from a high impact activity. This may include a collision during a contact sport such as American football, rugby, or judo. Motorcycle accidents may also cause knee fractures when the rider is flung from the motorcycle, resulting in crushing the knee. Weakened bones or diminished bone density can also predispose patients to an increased risk of fractures.
Causes
Several causes of knee fractures include:
- Falling down directly on the knee
- Receiving a powerful blow to the knee, such as during a car accident
- Severe and sudden muscle contractions that pull apart the patella
Symptoms
Some of the common symptoms of knee fractures include:
- Extreme pain in the knee
- Swelling and bruising
- Tenderness at the knee area
- Inability to bend or straighten the knee in an extended leg raise
- Muscle spasms
- Cracking or popping sound during movement
- Inability to walk
Torn Meniscus
A meniscus tear is another common knee injury reported by patients. Both your knees contain two C-shaped pieces of cartilage which serve as a cushion between your tibia and femur. This is called the meniscus
To understand how this injury arises, you first need to know what the role of the meniscus is. As mentioned, the menisci sit between the tibia and femur, stabilising the lower part of the leg against forces generated by your bodyweight. The medial meniscus sits on the inside of the knee while the lateral meniscus sits on the outside of the knee.
Essentially, the meniscus plays an important role in stabilising and distributing load in the knee joint. Meniscus tears occur when a patient twists or turns their upper leg while their foot is firmly planted and their knee is bent awkwardly. This can occur in activities such as dancing, cheerleading, snowboarding, or racquetball.
You should know that meniscus tears often occur with ACL tears, due to the nature of the knee twisting during the accident. According to a research study carried out by the Shelbourne Knee Centre, approximately 50% of patients with ACL tears also suffer from meniscus tears.
Causes
Causes of a torn meniscus include:
- Forceful twisting or rotating of the knee
- Sudden pivoting or turning when running
- Deep squatting or heavy lifting in the gym
In some cases, degenerative changes to the cartilage in the knee joint can also cause a meniscus sprain or tear with little trauma. This is due to the cartilage slowly losing its blood supply and resilience over time due to natural wear and tear. In other words, the risk of developing a torn meniscus increases with age.
Symptoms
The symptoms of a torn meniscus include:
- Intense pain in the knee joint, usually on the inside, outside, or back of the knee
- Swelling at the knee area
- Catching or locking of the knee joint
- Inability to bend or fully extend the knee
- Limping while walking
The pain may be bearable initially but will progressively worsen as inflammation and swelling begin to set in.
Knee Bursitis
Knee bursitis is an inflammation of the bursa. Bursas are the thin fluid-filled sacs that sit between your tissue, bones, and knee joint. Other joints such as the hips, shoulders, elbows, and ankles also have bursas which help to reduce friction between the bones and tissues.
Any one of the bursa in your knee can become inflamed, but knee bursitis most typically occurs over the kneecap or on the inner side of your knee. When these sacs become irritated, it fills with fluid, causing the sac to swell. This is your body’s natural defence mechanism against trauma to the knee by providing extra cushioning and support for the underlying bone.
Bursitis can occur due to repetitive movements which inflict trauma to the knee. One example of this is kneeling for extended periods of time, especially on a hard surface, resulting in pressure being applied to the knee area. Plumbers, roofers, carpet layers, coal miners, and gardeners have a higher risk of developing this condition.
However, knee bursitis is not as severe as compared to other knee injuries and usually goes away on its own. This may take up to a few weeks depending on the severity of the injury. The most important factor in the healing process is for you to rest as much as possible by giving the knee a break from whatever was causing the inflammation.
Causes
The causes of knee bursitis are:
- Frequent and sustained pressure on the knee, such as kneeling for an extended period of time
- Strenuous activity leading to overuse of the knee
- A direct blow to the knee resulting in mini-trauma
- Bacterial infection in the bursa
- Complications arising from osteoarthritis or rheumatoid arthritis of the knee
Symptoms
The symptoms of knee bursitis may include:
- Pain during activity, but no pain at night
- Swelling and inflammation at the front of the knee
- Tenderness at the affected area
- Bursitis caused by bacterial infection may produce pus as well as fever
Patellar Tendinitis
Patellar tendinitis, also known as jumper’s knee, is an overuse injury characterised by inflammation of the patellar tendon. Contrary to what its name suggests, the patellar tendon is actually a ligament.
To understand this injury, we first have to understand the role of the patellar tendon in the knee joint. The patellar tendon connects your patella to your tibia and works with the muscles in the front of your thigh to straighten your leg. Damage to this tendon can make it difficult to move around, hindering you from participating in sports activities.
Patellar tendinitis occurs when you overuse your knee joint, for example, when you jump and land repeatedly on hard surfaces. It is a type of sports-related injury commonly associated with elite athletes. With repeated stress and impact placed on the knee, your patellar tendon becomes irritated and inflamed from the minor strains and tiny tears. Basketball, netball, and volleyball players are more susceptible to this injury.
This leads to pain, soreness, and discomfort at the knee area, which may either be minor or severe depending on the extent of damage inflicted. If you continue to exercise or partake in physical activity with this injury, it may worsen over time.
Causes
The causes of patellar tendinitis are:
- Any kind of repeated activity which gradually damages the knee
- Sports that involve repeated jumping and landing, especially without bracing the knee properly
- Training on hard surfaces such as concrete
Physically active athletes who do a lot of running and jumping are more likely to get patellar tendinitis. Other risk factors include having tight quadriceps and hamstring muscles, which can increase the strain placed on your patellar tendon. Lastly, having a muscular imbalance can cause an uneven pull, resulting in tendinitis as well.
Symptoms
The symptoms of patellar tendinitis include:
- Pain between your kneecap and shinbone
- Tenderness to the touch at the affected area
- Tightness or stiffness at the knee area, particularly first thing in the morning
Arthritis
Many of us think of arthritis simply as an age-related disease that adults become susceptible to in their old age. However, did you know that arthritis as a disease actually comprises a complex family of over 100 types of musculoskeletal disorders?
Arthritis is a degenerative disease where inflammation and pain affect the joint as well as its surrounding tissues. The most common early signs of arthritis are typically observed in the back, knees, hips, and elbows. Depending on the severity of the condition, the pain and stiffness will vary.
There are four main types of arthritis:
- Osteoarthritis: The most common type of arthritis caused by a degradation of the cartilage in your joints over time.
- Rheumatoid arthritis: An autoimmune disease that can occur at nearly any age.
- Psoriatic arthritis: Usually observed in patients with psoriasis, an autoimmune skin condition.
- Gout arthritis: A type of arthritis due to deposits of uric acid crystals in a joint, typically starts in the big toe before moving up the foot and ankle joint.
In addition, post-traumatic arthritis can arise due to a sports injury or road accident. All of the different types of arthritis above affect the joints in different ways.
You should know that the damage sustained by the knee joint from osteoarthritis is irreversible. However, the symptoms of pain can be managed by receiving medical treatment, thereby slowing down the progression of the disease.
Causes
Osteoarthritis occurs when the cartilage that cushions your bones deteriorate over time. For this reason, osteoarthritis has also been referred to as a ‘wear and tear’ disease that tends to happen with older age. This wear and tear can be hastened by repeated impact injuries or bacterial infection.
Rheumatoid arthritis, on the other hand, is an autoimmune disease that has no known cause. The body’s immune system attacks the inside lining (synovial membrane) of the joint capsule, resulting in inflammation and swelling. It is thought to be due to hereditary factors that predispose patients to respond negatively to specific environmental factors.
Psoriatic arthritis also has no known cause for why the immune system attacks the joints and skin.
Gout arthritis occurs when urate crystals accumulate in the joints, causing inflammation. This happens when you have high levels of uric acid in your bloodstream.
Symptoms
The general symptoms of arthritis include:
- Pain
- Stiffness
- Swelling
- Redness
- Decreased range of motion
Injury Prevention Strategies
Injury prevention may sound boring, which is why most athletes and sports enthusiasts tend to not give it the much-needed attention it deserves. After all, we never expect injuries to happen to us until it finally does, exposing the false sense of invincibility we’ve allowed ourselves to believe in.
The truth is, knee injuries occur all the time, whether at the professional, collegiate, or recreational level. This can cause a myriad of problems, especially when your busted knee leaves you sidelined for months. Injury prevention techniques thus become paramount for protecting your knees and ensuring that you get to continue enjoying your favourite sporting activities. After all, an ounce of prevention is worth a pound of cure.
Targeted Strength Training
When we think about how to strengthen the knees, we must first think of the muscles surrounding the knees. This means the quadriceps, the hamstrings, the glutes, and the hips. To prevent injury, we need to focus on strength endurance, rather than maximal strength. For those who are physically active, you also need to consider the years of jumping and running with incorrect form. This can cause inflammation of the tendons and wear away the cartilage.
Imbalance is the keyword here. You should know that your abductor muscles are responsible for moving your leg away from your body’s midline, while the adductor muscles are responsible for moving the leg towards your body’s midline. Should your adductors be stronger than your abductors, your knees will cave inwards, creating the valgus knee. This is not a strong position to be squatting or landing from a jump in, and can easily cause injury.
A spring can’t work properly unless it lands exactly straight. One of the best ways to fix this issue is to fix the glutes. The gluteus maximus is responsible, amongst other things, for the external rotation of the hips. Most importantly, it helps to keep the leg pointing forward during running.
The gluteus medius meanwhile, is the prime mover when it comes to hip abduction, moving the legs apart. The gluteus medius likewise is a hip abductor. Together with other muscles like the tensor fascia latae (TFL), these muscles help to keep the knee straight and hips balanced when you’re standing on one leg. This can also help to prevent iliotibial band (IT band) pain. The IT band originates at the crest of the pelvis, above the hip, and runs to the outside of the knee. It’s attached to the gluteus medius quadriceps and hamstrings.
Problems occur when an individual spends all their time running in straight lines, strengthening these muscles in the sagittal plane but don’t incorporate any side to side hip movements into their training. Again, running isn’t the problem. Just running is the problem.
In order to strengthen the muscles supporting your knee, you should do the following exercises.
#1 Hip Abduction
Hip abduction exercises can help strengthen the hips effectively.
To begin, lie on one side and raise the leg into the air. Complete 3 sets of 15-20 repetitions in a slow controlled manner. Use a resistance band if you need to.
If you find this hard, there’s a good chance that hip weakness is a contributing factor to your knee pain. This exercise can also be effective for re-activating the hip abductors and improving awareness of the muscle so that you use it more during movements.
#2 Glute Bridges
Lie on your back and bend your knees, extending your hips upwards with your feet remaining flat on the floor. Drive into the heels of your feet and lift your hips up as high as possible, holding for a moment at the top and squeezing your glutes. Lower down slowly and repeat for 10-15 repetitions at a go. In order to increase the difficulty of the exercise, you can elevate your starting position by performing it off a bench. You can also add weights onto your hips to increase the load.
Lying on your back enables your hips to be the primary mover of this exercise, which isolates your glutes without overly engaging your knees. The importance of developing the glutes for knee injury prevention cannot be emphasised enough, as the gluteus maximus muscle is directly involved in decelerating stress to the knee and helping reduce pain and injury to the knee joint.
#3 100 Up
This exercise was created by Walter George who used the technique to become an unbeatable long-distance runner. He also broke the world record for the fastest mile in 1886. The 100 Up involves running or marching on the spot with high knees, bringing them up to your chest on each repetition. We’re aiming for high volume here, as the name suggests, we want to perform 100 repetitions on each side.
But you should build up to that if it’s too much to begin with. If you’re in pain, you can perform this movement by slowly raising one foot only once the other is placed on the ground. You can also hold on to something for balance. As you do, focus on keeping the hips aligned and ankles straight as you return the foot to the same place every time. The goal is to move in alignment with each step even as you begin to feel fatigue. This will also help develop the hip flexors.
#4 Steady-State Running
As paradoxical as it may sound, running actually helps to protect your knees. Although it is true that sprinting and repeatedly landing on hard surfaces will wear out the cartilage in your knee joints over a long period of time, you can avoid this by dropping the intensity. Low-intensity steady-state running will actually help to lower your risk of knee injuries by building up your leg muscles.
In all my years treating knee injuries, I have always recommended steady-state running as a part of anyone’s physical exercise routine. Beyond just strengthening the heart, helping to lower blood pressure, aiding recovery by encouraging circulation, and improving cardiovascular endurance, running is one of the most functional and fundamental movements there is. Running teaches you to move and use your knee joint properly. Even if you only run once a week, you’ll feel the benefits in strengthening your knee.
Correct Muscular Imbalances
One thing you should know about the human body is that the muscles and joints work best when your body is in alignment while moving. The importance of postural alignment and muscular balance forms the foundation of your performance during physical activity. If there are muscular imbalances causing your movement patterns to become misaligned, it sets you up for a higher risk of injury.
Muscular imbalances can arise when certain overused muscles become stronger than other less active muscles. This leads to the stronger muscles overcompensating for the weaker muscles, which causes fatigue to build up easily. For example, athletes who are more quad-dominant tend to have very strong quadriceps muscles but weak hamstring muscles. This affects their running style, walking gait, and also leads to the development of bad postural habits.
The knee becomes very susceptible to an overuse injury when you have a pre-existing muscular imbalance. For example, weakness in the hamstring muscle group can put you at a higher risk of suffering an ACL injury. Limited flexibility and tightness in the hamstring muscles due to weak quadriceps femoris muscles can also lead to anterior knee pain, due to the increased compressive forces placed on the patella.
Muscular imbalances might also change the path of motion for your knee joint during movement. For example, the knee might be pulled to one side or the other instead of staying aligned due to a muscular imbalance between the quads, hamstrings, and hips.
Most people are either unaware of their muscular imbalances or deliberately ignore them until it becomes too late. But if you want to bulletproof your knees and lower your risk of injury, you should focus on achieving balanced muscles and, by extension, good postural alignment. The best way to do this is to do isometric work, which involves single-leg exercises that target the quads, hamstrings, and hips.
Do Isometric Work
Isometric exercises produce a muscle contraction without actually moving the joint. Imagine holding a pair of dumbbells with the arms flexed or sitting fully in the bottom of a squat position. These exercises are commonly deployed by physical therapists for rehabilitation programmes but are often overlooked by fitness buffs.
The isometric exercises that I recommend include:
- Nordic Hamstring Curl
- Single-Leg Bulgarian Split Squat (with the rear leg elevated)
- Single-Leg Romanian Deadlift
- Single-Leg Hip Thrust
For each of these exercises, hold the contraction position for 30 to 60 seconds before repeating for a few sets. In the Nordic Hamstring Curl, for example, holding the position at around 45 degrees should get the hamstrings firing. You will notice that I have also included single-leg exercises that you can incorporate into your prehab routine. This is to ensure that there are no muscular imbalances between the left and right legs.
Flexibility Work
Flexibility is one of the most neglected aspects of training when it comes to injury prevention. However, we didn’t always have to put in so much effort to have good flexibility. Think back to when you were younger and how much more active you were back then. Children are most flexible and are able to do splits, with toddlers even being able to put their feet in their mouths.
This innate flexibility and mobility slowly diminish as we age. Many individuals live a sedentary lifestyle and develop poor postural habits. Others who exercise frequently neglect the importance of a good warmup and cool-down stretching routine, leading to a loss of flexibility.
Believe it or not, your limited flexibility, no matter how inconspicuous or unimportant it may seem, lies at the root of so many injuries. In sports especially, most injuries occur because the body wasn’t ready for it.
I recommend the following exercises as part of a dynamic stretching routine.
#1 Toe Taps
Standing tall, kick one leg up and touch your toes to the palm of your hand. Alternate between your left and right leg and repeat 10-15 times on each side. If you can’t reach all the way up to your hand, simply extend your leg as far as you can each time.
#2 Reverse Lunge And Hop
Step back with one leg and sink into a lunge position. Then swing the back leg forward until you raise your knee all the way up to where it forms a right angle to your chest. Maintain an upright body position and repeat on the other side. Perform 10-15 repetitions on each side.
#3 Standing Roll Downs
Stand with your feet about hip-width apart. Let your arms dangle. Slowly roll your head down your body as you bend forward until you reach your maximum distance without having to bend your knees. Ideally, you should aim to touch the ground with your palms. Slowly roll back up one vertebrae at a time. Repeat 10 more times.
#4 Sideways Leg Swing
While facing a wall or holding a handrail for support, swing one leg at a time from side to side in front of your other leg. Try not to let your torso rotate as you perform this stretch, and keep an upright body posture. Swing both legs 20 times each.
#5 Lateral Lunges
With your hands on your hips, take a big step to the side and perform a squat. Lean to that side while straightening out the knee of the opposite leg. Stick your butt back, keep your weight on your heels and keep both feet pointed straight. Then, switch sides and lean towards the opposite side, squatting down before stepping back up to the centre. Perform at least five steps to the left and five steps to the right.
Exercise And Weight Management
The benefits of a healthy exercise routine for weight management:
- Reduces pressure on the knees
- Reduces inflammation in the body
- Reduces the risk of chronic disease
- Lowers uric acid levels and the chance of gout arthritis
- Slows down cartilage degeneration in osteoarthritic knees
When it comes to overuse injuries brought about by gradual wear and tear, one of the best things you can do for your knees in the long-term future is to lose weight. In fact, when it comes to arthritis, losing weight pays big dividends in terms of pain relief.
Medical researchers estimate that for every step you take, an additional force of 3 pounds is placed on your knees for every additional pound you gain. In other words, losing 10 pounds will result in 30 pounds less pressure per knee on every step. This difference is further amplified by the number of steps you take each day, with the average person taking around 5,000 to 6,000 steps a day. 5,000 steps and 10 pounds of body weight will generate 150,000 pounds of pressure on the knees each day, which makes for a staggering difference of 54 million pounds of pressure across one entire year.
This means that losing 10 pounds can make a difference of 54 million pounds of pressure applied on your knees each year.
Conclusion
The best way to deal with knee injuries is to stop them from happening in the first place. It’s time to start rethinking our training and the steps we take towards injury prevention. Think of avoiding injury as one of the main training objectives that you aim to achieve. Even if you’re not an athlete, you will still benefit from bulletproofing your knees.



